What is the treatment with PPP and the preparation of platelet-rich plasma?

What is a platelet?
Platelets are dyslexic and non-nucleated blood cells that play a role in many different yard functions, such as homeostasis or blood coagulation, antimicrobial inflammation, host angiogenesis, and wound healing
Although primarily focused on the role of platelets in blood coagulation, it soon became apparent that there were more than 1100 proteins present in the platelets, including growth factors, immune system signals, enzymes and other biological compounds that were restored at different stages of the process The tissue is involved. The platelet-rich plasma or PRP is a blood product that is produced during the process of separating fresh and unclad blood.
Years ago, platelet-derived products have been prepared in blood transfusion organizations, and have been used in hospitals and medical centers to bury or prevent bleeding in patients with plurality of platelets or disorders. It is also used as a preventive treatment in cases of reduced platelet production in bone marrow, invasive surgery, active hemorrhage, and so on.
Thinking of using platelet products in other therapies has been based on the theory that hard and soft tissue repair is performed by specific proteins and a process of intracranial and extracellular responses that are now fully understood. But what is certain is that the platelets play a prominent role in activating processes and the production of growth factors and specific proteins.
Platelets, in response to tissue damage and vascular perforation, result in platelets and platelets, resulting in homeostasis, and then by secretion of certain proteins, proliferation and cellular differentiation, removal of damaged tissue, the formation of extracellular vessels and matrix, repair and repair of damaged tissue Cause.
In recent years, with the advancement of medical knowledge of PRP in various medical fields such as cosmetic surgery, plastic surgery, jaw surgery, oral surgery. Heart surgery, neurosurgery, orthopedics, sports medicine, ENT, dentistry, burns and so on. In this method, by using the technique of plasma separation and platelet condensation from the blood of one, it is used by the individual for himself and as a new and new method is introduced into the world of medicine.
What is the preparation of platelet-rich plasma?
Procedures and certain substances for preparation of PRP with a concentration of at least 1 million platelets in a volume of 5 ml are necessary because they are mainly composed of red blood cells, white blood cells, platelets and serum.
Red blood cells are needed for oxygen and nutrition of the cells, although red blood cells are stagnant, lactic and PH reduced, which is likely to be lost in living bone cells.
In a study by MARX, cysteine Ileak osteoblasts were inhaled and 90% saline was stored. After 3 hours, 97% of the bone marrow cells stored in 90% saline were still alive, while only 85% of the cells that kept the blood were alive.
The stagnant red blood cells in the bloodstream of the vein or the usual clot are blood vessels that block the cells of the bony cells. When blood clots form, 93% of the clots form red blood cells, 6% of platelets and less than 1% make white blood cells.
Compared with the PRP clot, 93% platelets, 5% red blood cells, 1% white blood cells.
The first round in the centrifuge technique is the removal of red blood cells from the plasma, which include white blood cells, platelets, and coagulation factors.
In the second round, the platelets and red blood cells are separated from the plasma and produce PRP. When the plasma is physically separated from PRP, it becomes a low-density plasma.
One-way techniques do not effect the removal of PRP from the platelet and produce very few platelets.
The higher the number of platelets collected, the greater the growth rates.
PRP factors have a threshold for altering the bone and the soft tissue repair stages. There is no clinically different result when the threshold is not reached. Unfortunately, the threshold of change in the stages of recovery in a person is different from that of a person.
The higher the concentration, the greater the change in the repair speed, and the lower the platelet concentration, the fewer changes.
Usually, for dental work, 20 to 60 ml is taken to produce sufficient PRP from the patient.
When PRP is ready for use, it should be used at the time of use, because once it is activated, the platelets immediately begin to secrete growth factors.
90% for the first 10 minutes and 100% for 30 minutes, so an anticoagulant, such as dextrose citrate, enters the blood when taking blood from the vein, which may prevent PRP from coagulating for 8 hours. Although PRP is best used when it is produced within 1-3 hours.
PRP is not a defensive barrier. The defensive barrier prevents soft tissue invasion of the site for at least weeks or months.
PRP does not prevent fibrolas invasion for a long time into the site of the transplant.
Although it may be used in this defense bar, because fibrinogen also has beneficial effects on soft tissue, it acts as a hemostatic agent and has the ability to reduce postoperative edema and pain.
When PRP is added to the bone, bone formation increases in terms of speed, quality, and volume.
Today, it's unclear to anyone that the platelets trigger and accelerate collagen repair, elastin, and intercellular matrix, and ultimately lead to happiness and a sense of superiority in young people.
Because of this, it is a congested plate for treating wrinkles in the face and neck, treating blurry and numbness under the eyes, removing frown lines or laughing, treating wrinkles in the back, controlling and treating hair loss, scarring or surgical swabs, and Burns, accelerates the recovery of jaw and facial injuries, treats and torsions in athletes and reduces the period of rest, especially in the world of professional and championship sports.
PRP has been accepted as a way of introducing a high concentration of growth factors and other biochemicals into the damaged tissue to optimize the tissue repair environment. However, all PRP products are not similar. Total blood volume taken from the patient. Efficiency of platelet extraction. The final plasma volume in which the platelet is suspended, the presence or absence of white blood cells or red blood cells, and the addition of thrombin or calcium chloride for activation can all affect the characteristics The final product of PRP is affected.
Clinical Effects of PRP Implants on Bone Health
The bone health and integrity of the dental implant result from cell migration, differentiation, production and bone reshaping at the levels. All of these processes are dependent on blood platelets and coagulation. Therefore, PRP can be used to increase the bone health of elderly patients, people with diabetes, osteoporosis or other forms of bone repair or in cases of posterior maxillary disturbances.
PRP in dentistry has been successfully used for two decades. PRP can be used in some dental treatments including implant placement, periodontal bone surgery, soft tissue surgery and jaw reconstruction.
For example, a dentist who is going to perform a dental extraction surgery can use PRP to improve the wound after tooth extraction. It is very important that the wound heals after removing the teeth, because dental implants can be placed without any problem. When inserting an implant, blood clot or PRP, the inside of the hole, the implant surface and the surface of the bone, and Covers the metal.
When an implant is used, despite the fact that there is a complete macroscopic contact between the metal and the bone, there are microscopic holes between the metal and the bone that form blood clots in this space. Microplatelets, red blood cells, white blood cells and cell adhesion molecules such as fibrin, fibronectin, and vitronectin are usually found in the microscopic space between the metal and the bone. In this situation, cell adhesion molecules play an important role in covering implant surfaces and bridging Between the surface of the implant and the bone.
The bone health model shows that the surface of the implant, the cavity around it and the bone cavity surface of the osteoblast implant covering the bone surfaces, red blood cells and platelets are worn.
The lactates secrete seven growth factors after they have been degranulated. These growth factors bind to the surface of the membrane of osteoblasts, which activate them by stimulating cell proliferation, migration, production of 3: 4, bone maturity, and ultimately bone wall binding To the surface of the implant. As a result, osteoblasts and stem cells of the brain and bone multiply in the bony wall of the perforated area and migrate onto the fibrin strands and other cell adhesion cells that are in this space.
By migrating these cells onto fibrin strands, the brain and bone cells of the fibrin fibers are separated from the implant surface. Fibrin binds to implants with better tissue surfaces and more bone health than these implants. Once the cells of the brain and the bone migrated along the fibrin strands, they produce differentiated osteoids, which are seen in the examination of implant histology.
Histological examination confirms the events described, note that stem cells produced an octahedron from the osteoid to the left side of the implant.
A number of osteoblasts are located on the edge of the osteoid edges, and some of them are trapped within the osteoid to become adult osteitis. The remainder of fibrin strands are between the osteoid motions. This migration sequence is often misunderstood for differentiation and bone production.
This image that osteoblasts on a string of fibrin forward and is left in the form of a snail that leaves a trap behind it is false, in fact, the growth of the chain is more correct. A stem cell that is migrating is multiplied and differentiated into osteoblasts. Then, stopped migration of osteoid secretion involves osteoblast and it becomes osteositis.
The female cell derived from the split cell forward is now split into a cell to produce another girl. This process is repeated until the edge of the bone reaches the implant, and then the same process continues on the implant surface, only The difference is that this process is not directly applied to the metal surface of the implant, but on the fibrin connected to the surface of the metal.
Once again, the understanding has shown why implants with tissue levels have a higher bone contact surface because fibrin is more readily connected to these levels, and the importance of other cell adhesion molecules in better bone health is better.
Studies from DAVIS and colleagues showed that the actual bone is not directly in contact with the metal surface, but the cement that is commonly seen on the Van Ebner lines is in contact with the metal surface. This process is similar to the process of bone reshaping, in which osteoblasts produce cement that is placed on mature bone surfaces and connects the new bone to prevent it from separating it.
The bone attachment process also depends on the cement that binds the new bone to the implant surface. Natural bone from collagen strands of the type 1 Among them, crystals 6:18 have been composed of small amounts of growth factors BMP2G, but cements have been made of sialoprotein and osteoporosis, among them calcium hypoxophosphate crystals.
This bioactive cement flows through the gaps, cavities and grooves of the implant's surface, because ghavami resembles toothpaste, as it does in the form of unstained plaster dough. With the hardening of the cement when crystals of calcium Haypvfsfat form osteoblasts collagen fibers and osteoid added to it, such as steel wire string collagen and new bone to cement connects so the process of accession bone The cement with a diameter of 5 mm adheres to the implant and attaches it to the actual bone. This sequence of processes from initial cell proliferation, cell migration, cellular differentiation, production of osteoid cements all begin with, and depends on, growth factors derived from platelets.
PRP effects on bone repair using bone replacement materials
Since the use of PRP for bone and soft tissue repair has benefited, it is thought that the benefits of its use depend on the presence of autologous transgenic cells and will only be useful in autoimmune grafts. However, recent studies have shown that PRP can be restored with Improve the use of bone substitute materials.
Despite the claims, no bone substitute or allogeneic bone products in humans have led to bone growth. Even the mineralized or inorganic allogeneic bone does not have sufficient concentration of BMP to induce the growth of a new bone in humans, so today the material Bone replacement is dependent on bone marrow transplant bone precursor cells to guide bone growth.
The mechanism of action of these products can be seen in the placement of bone replacement materials in the sinus graft. In this condition, particles of bone substitute material are usually placed in the sinus space under the membrane of the bone. These particles are immersed in blood clots containing fibrin, fibronectin, red blood cells and white blood cells, and plenty of platelets. If the PRP clot exists, the platelet count will be 4-7 times.
In 10 minutes after the development of a dense ganglia of platelets, they release 7 growth factors. Some of these growth factors affect blood vessels, bone marrow and sinus membrane to induce growth of the capillaries into the graft. Other factors affect on the inner and outer surfaces of the bone wall and the sinus roof, and begin migration, cell differentiation, and bone formation as the process of bone implantation.
As seen in the bone attachment model, bone precursor cells grow along the fibrin network between the bones and the bone substitute particles and bind them together. The fibrin binds the bone substitute particles together. Bone precursor cells migrate along the surface of fibrin strands and produce bone cement, so as the hyroxyapatite coating, on the surface of dental implants, bone-exchange particles eventually join the bone.
The bony network that surrounds these particles binds them to a bony wall to create a stable bond. Since bone formation processes involve the secretion of growth factors and cellular stimulation, cell migration and differentiation have not been performed before. Compared with autologous bone graft with a large number of differentiated cells in it, bone formation in cases of use Substitute materials will be taken later and the bone will be created at a lower rate. PRP can stimulate bone production in a shorter time.

People who viewed this page also visited:
What are the dental implant treatment stages?
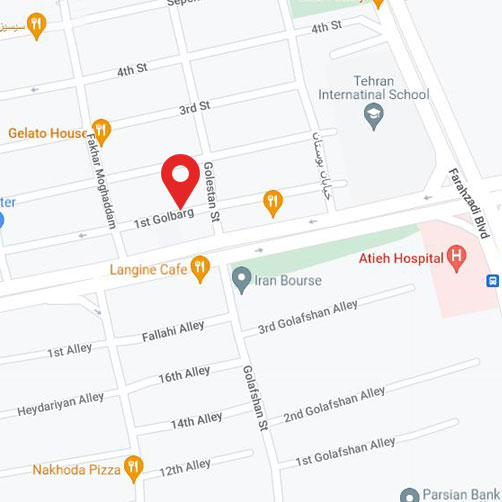
Implant Professional Center in Tehran
The best implant expert in Tehran
The best implant center in Tehran
What is immediate loading of dental implants?
Implant problems and implications
Force direction and its relationship with the implant body design
Unsuitable cases for dental implant
The geometry of the implant and its relationship with occlusal forces
The relationship of the implant body and functional surface